Equine
History of the Horseshoe Part 1
If it were not for the horseshoe and wagon wheel, the United States would not have been founded, according to Lee Liles. The owner of the National Museum of Horse Shoeing Tools and Hall of Honor said Oklahoma is the grandest example in the world.
Horseshoe books date back to 400 B.C. In fact, the oldest horseshoe at the museum in Sulphur, Okla., is more than 500 years old from Denmark.
“I don’t like going back much farther than 1860 because we don’t have the documentation to back it up,” Liles explained. “You got a few magazines like the Harper Weekly and the Wallaces’ Report, but you want to verify the facts.”
19th Century Patents
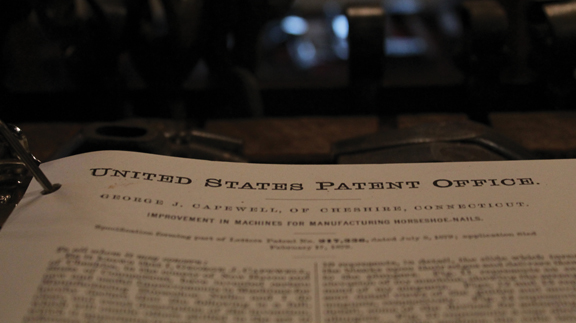
The first patent on a horseshoe manufacturing machine in the United States was issued in 1834 to Henry Burden, a Scottish-born industrial engineer. By 1850, Burden had more than 50 different patents on his machines at Burden Iron Works in Troy, N.Y., Liles added.
This was all before the first horseshoe nail patent, which was issued in 1863 to Daniel Dodge in Keeseville, N.Y. The horseshoe nail is the most difficult nail in history to manufacture, Liles explained.
“It’s got a lot of different tapers to it,” he explained. “The nail needs to be strong and durable enough to drive through a foot, come out, be turned over 180 degrees and clenched down in the horse’s foot.”
The nail industry has changed a lot throughout the years, Liles said. In 1853, the horseshoe nail was made from Swedish Iron, but copper nails have become popular in recent years. The oldest nail company left in the United States was the Capewell Horse Nail Company owned by the Mustad family. The nail company started in 1881, and they recently moved out of the country.
“All of these major shoe companies, tool companies and nail companies were located in the northeast United States,” he explained. “That’s where the population was. There weren’t any companies located down here in the South like Oklahoma or Texas.”
Horseshoeing Literature
Most information on horseshoeing actually came from Germany, Liles explained. German books were first written in 1861 by Leisring and Hardman. In 1882, Lungwitz was added as a co-writer.
“[Leisring, Hardman and Lungwitz] were the main vets at the Royal Veterinary College,” Liles said. “[Hardman] wrote his own first book in 1884 and wrote 24 editions. Nobody else has ever written that many books.”
Liles said books are the greatest assets for education. In 1866, the U.S. Congress adapted the cavalry books would be written on the Dunbar System.
“Alexander Dunbar was a person who our Federal Government paid to teach anatomy to horseshoers back in that era,” Liles explained.
John Kerman, who was running a horse shoeing school at Fort Carlisle, Penn., wrote the book written on the Dunbar System. The first American horseshoe book was written in 1871. In 1902, Kerman came to the shoeing school at Fort Riley, Kan.
“The cavalry has been the main source of horseshoers in this country up to the 1950s,” Liles said. “The Army technical manual, TM-220, has been the most copied horseshoeing book in history.”
In the 1890s, Pennsylvania State recruited Mississippi-native, John Adams as a professor. The university sent Adams to Germany to study under Lungwitz.
“When he came back in about 1896, he and Lungwitz were such good friends that he had permission to write the American edition of the Lungwitz book,” Liles explained. “When he came back, Adams brought an instructor from Germany to Penn State to teach anatomy and horseshoeing to the vet students.”
Even Cornell University and Michigan State University had a protégé of Lungwitz in 1913, Liles said.
William Russell
“We had a great educator in Cincinnati, Ohio, who wrote 15 horseshoeing books from 1879 to 1907,” Liles explained. “His name was William Russell.”
In 1887, the first shoemaking contest was held in Cincinnati, Ohio, where Russell won. “The contest consisted of making 100 shoes on an opry stage in front of 3,000 spectators,” Liles explained.
Russell made 100 horseshoes in two hours and 40 minutes with the help of a team. John Silk, who later became a famous horseshoer, was one of Russell’s competitors.
In the 1890s, many horseshoers, including Russell, created display cases filled with their horseshoes. Many of these display cases are still intact and hanging in the museum. One of the cases was in the World Fair in St. Louis in 1904.
“When it went to the World Fair, they added nails to the case,” he added. A photo of the case at the World Fair was added into one of Russell’s books, and it was one of the last display cases he made. Russell offered all of his collection for sale in the same year.
“He died in 1907,” Liles explained. “He was a sick man, and he was blind when he died.”
Aluminum Horseshoe
Liles also has a case located at the museum built in 1895 had an aluminum horseshoe inside. “That is very rare,” he said. “In that era, they only produced 65 pounds of aluminum per year. Aluminum was a precious metal, and you had to buy it through a jeweler.”
Liles said he does not think the aluminum held up well to wear and tear. William Wedekind received the title, “The World’s Greatest Horseshoer” at the 1892 Chicago World’s Fair. Wedekind even made an aluminum horseshoe in 1883.
“It was so light that it floated on water,” Liles explained. “They can’t duplicate the shoe today to make it float on the water.”
The Right Shoe
Liles said when people come to museum, they are used to dealing with one breed of horse and one discipline with the horse. The type of horseshoe used depends on the breed and the discipline. “In this country, we have roughly 400 different breeds of horses,” Liles said.
Liles said he was a horseshoer, which is a lot different from a cowboy shoer. For instance, a horse that is going to go trail riding or ranching needs a high-quality steel horseshoe.
A show horse will wear aluminum shoes because the aluminum will wear the toe quicker. “It will give him a quicker time to break that shoe in,” he added. “If your shoe isn’t new at the show, he has to get that shoe back to where it feels comfortable.”
Many of the plastic shoes are meant for horses that are on concrete, asphalt or wood. Liles said plastic shoes are commonly used in the circus.
A common misconception is people think the weight of the horseshoe affects a horse in either racing or working. “They think plastic is so much lighter,” he explained. “If that is the case, why don’t you just ride him barefoot?”
To learn more about the history of the horseshoe, visit www.horseshoeingmuseum.com.
This article was originally posted in the July 2016 issue of Oklahoma Farm & Ranch.
Equine
Grain Overload in Horses
By Dr. Devon England
You come home after a long day at work, and your feed room door is wide open and grain bins are empty. What do you do? Before you call your vet, figure out what grains were eaten, try to estimate how much and determine which horse or horses got into the feed. Did your horse just get into some hay or alfalfa pellets, or did he get into a high sugar grain like Omolene 300? Did your horse get into chicken or cattle feed? If he did, is it a medicated feed, containing an ionophore like monensin or lasalocid?
Grain overload is an emergency, with better outcomes, the sooner the horse is treated. So, call your veterinarian as soon as you figure out a possible grain overload has occurred. Based on what feed and how much feed your horse consumed, your veterinarian can try to determine the risks to your horse and come up with a treatment plan. Signs of grain overload include colic, lethargy, inappetence, diarrhea and lameness. These signs will vary depending on how long ago grain ingestion occurred and the severity of grain overload.
If your horse got into hay or alfalfa pellets, these are low in sugar and therefore not a high risk for problems. Your horse may just have a mild belly ache (colic) episode. If your horse got into a feed like Omolene 300, they are at risk for grain overload. How severely they are affected will depend on a few factors including how much grain was eaten (5lb vs 30lb), if the horse normally receives that grain or doesn’t receive any grain, and the size of the horse vs the amount of grain eaten. Eating 5lb of grain for a full-size horse who normally receives grain may not be a problem, but that same amount of grain eaten by a small pony who normally only receives hay will be a problem.
Treatment for grain overload should be initiated as soon as possible. This includes lavaging the stomach to remove any remaining grain. Stomach lavage is only successful in removing feed within the first couple of hours. Horses will be given mineral oil or charcoal to decrease absorption of breakdown products (acids) from grain fermentation and protect the intestinal lining from damage. Intravenous fluids are given, because horses can quickly become dehydrated with grain overload, due to digestion products from the grain drawing in a lot of water into the colon. Anti-inflammatories, lidocaine, and ice boots are used in more severe cases to decrease the risk of laminitis. In more severe cases with damage of the intestinal lining, antibiotics may be used to prevent infections associated with bacterial escape from the damaged intestine.
If your horse got into medicated feed containing an ionophore, your horse is at high risk for heart failure and muscle damage, on top of grain overload. Ionophores are toxic at very low doses in horses (2mg/kg). These drugs are added to livestock feed to decrease parasites (coccidia), to help with feed efficiency, to decrease risk of bloat and to decrease methane emissions. If your horse has eaten ANY amount of medicated feed, they should be immediately seen by your veterinarian, even if they are not showing any clinical signs. Horses can have no clinical signs or be mildly lethargic in cases where small amounts of medicated feed were eaten but still have evidence on blood work or muscle and heart damage. Clinical signs include initial inappetence or colic signs, weakness or neurologic signs in the hind end, muscle fasciculations (twitching), laying down more, and not being able to stand. There is no anti-dote to ionophore toxicity. Treatment may include mineral oil, IV fluids, anti-inflammatories and supportive care, depending on how soon toxicity is identified. In severe cases, horses can die or develop heart failure, necessitating euthanasia. In less severe cases, especially if identified and treated early, horses can recover fully.
Grain overload can come with serious complications if severe or medicated feeds are involved, especially if treatment is delayed. Secure your feed room as best as possible and keep medicated livestock feeds in a separate location to prevent cross-contamination. And if you have any concerns about your horse getting into feed, call your veterinarian as soon as possible.
This article was originally published in the February 2025 issue of Oklahoma Farm & Ranch.
Equine
Gastric Ulcers

By Dr. Devan England DVM
Does your horse have gastric ulcers? Gastric or stomach ulcers are frequently blamed for a variety of things including poor performance, acting ‘cinchy’, weight loss, not eating, poor coat condition, diarrhea and colic. However, gastric ulcers are not always the culprit and the only way to know for sure if your horse has gastric ulcers is to look at the stomach on camera, using an endoscope. Poor appetite and poor body condition are the mostly widely observed clinical signs with gastric ulcers, however, these are non-specific. If you think your horse might have gastric ulcers, the best place to start is to talk to your veterinarian and consider scheduling a gastroscopy. Gastroscopy requires the horse be held off feed for at least 16-18 hours and held off water for at least 6-8 hours. Fasting off feed and water is necessary to allow the veterinarian to see the whole stomach. If restricting feed or water is difficult in your management situation, many veterinarians will allow you to hospitalize your horse the night before gastroscopy for proper fasting.
Gastric ulcers are split into two types, classified by the location of the ulcer in the stomach. Squamous ulcers are ulcers that occur in the squamous or skin like portion of the stomach. This is the top part of the horse’s stomach, is closest to the esophagus, and has squamous tissue to protect this portion of the stomach from stomach acids. The other ulcer type are glandular ulcers. Glandular ulcers occur in the bottom portion of the stomach, which is closest to the small intestine. This portion of the stomach has glandular mucosa with cells responsible for producing stomach acids for digestion as well as cells that produce mucus and buffers to protect the lining from stomach acid. Gastroscopy is important not only for diagnosing whether ulcers are present but also determining the severity and the type of ulcer, because these two ulcer types require different treatments.
Squamous gastric ulcers are common in racehorses both in and out of training, with higher prevalence in racehorses under training. Prevalence in Thoroughbred racehorses in training has been reported to be up to 100% (Sykes 2015). Squamous ulcers are also prevalent in Western pleasure horses, Thoroughbred stallions on breeding farms, and Italian donkeys (Sykes 2015). Glandular gastric ulcer prevalence has not been as well described as squamous ulcers. Glandular ulcers are reported to be most common in Thoroughbred and Standardbred racehorses, Canadian showjumpers and polo ponies, and American Quarter Horses (Sykes 2015).
Risk factors for ulcers vary by ulcer type. Anti-inflammatories (Bute, Banamine) can increase the risk of glandular ulcers in some horses by affecting normal defense mechanisms but are not a high risk in most horses. Horses that display stereotypic behaviors, such as cribbing, have an increased risk of squamous ulcers. Grain fed before hay in non-exercising horses, feeding larger amounts of grain, and increased time between meals increases the risk of squamous ulcers. Increased time with high intensity exercise and housing in single pens is associated with increased risk of glandular ulcers. A straw only diet, lack of water access and lack of direct contact with other horses increases the general risk of gastric ulcers.
If your horse is diagnosed with ulcers, the mainstay of treatment is a buffered formulation of omeprazole (Gastrogard, Ulcergard). Over the counter Omeprazole and compounded Omeprazole are not effective because without buffering, the acidic stomach quickly breaks down the drug before absorption. Most horses with squamous ulcers will have healing of these ulcers after a 4-week course of Gastrogard or Ulcergard at treatment dose (whole tube for the average horse). Some horses may be healed by 3 weeks of treatment, but all horses should undergo a recheck gastroscopy before stopping treatment. Horses diagnosed with glandular ulcers need combination therapy with Gastrogard/Ulcergard and Sucralfate for 4 weeks. About 2/3 of horses with glandular ulcers will heal in this time, but some horses may require longer treatment times so a recheck is always recommended before discontinuing treatment.
Horses at higher risk of gastric ulcers may benefit from preventative (low) doses of Ulcergard (1/4 tube in average sized horse) given for a few days before and during high stress situations like long distance travel and competitions. Sea buckthorn berry supplement may be protective against formation of glandular ulcers. Dietary management to decrease the risk of ulcers includes providing more frequent small hay meals if pasture access is not available, limiting high sugar grains as much as possible and adding vegetable oil to the feed.
Sykes BW, Hewetson M, Hepburn RJ, Luthersson N, Tamzali Y. European college of equine internal medicine consensus statement – equine gastric ulcer syndrome in adult horses. J Vet Internal Med 2015; 29:1288-1299.
Equine
Meeting the Nutritional Needs of Older Horses

As horses age, their nutritional needs change significantly, necessitating careful adjustments in diet and management to maintain their health and quality of life. Older horses, often categorized as seniors around the age of 20, may face a variety of age-related challenges, including decreased digestive efficiency, dental issues, and metabolic disorders, all of which require tailored nutritional strategies.
Challenges and Considerations for Senior Horses
One of the primary challenges in feeding older horses is their reduced ability to digest and absorb nutrients. As horses age, their digestive systems become less efficient at processing essential nutrients like proteins, vitamins, and minerals. This decline can lead to conditions such as muscle loss, weight loss, and decreased immunity, making it crucial to adjust their diets to meet these changing needs.
Dental health is another significant concern. Many senior horses experience dental issues, such as worn or missing teeth, which can impede their ability to chew and digest forage effectively. For these horses, switching to a senior complete feed—formulated to be highly digestible and to meet all of the horse’s nutritional needs—can be beneficial. These feeds are designed to replace forage entirely when necessary, ensuring that even horses with severe dental problems can still receive a balanced diet.
Management Strategies
In addition to dietary changes, proper management practices are essential for the well-being of senior horses. Regular veterinary check-ups are critical to monitor their health and detect any early signs of age-related diseases. Common conditions like Cushing’s disease and metabolic syndrome can have a significant impact on a horse’s nutritional requirements. For example, horses with metabolic disorders may need a diet low in sugars and starches to prevent spikes in blood glucose and insulin levels.
Moreover, older horses often require adjustments in their living conditions to reduce stress. As they age, horses may become more sensitive to changes in their environment, such as temperature fluctuations or alterations in their social groups. Ensuring a stable, comfortable environment with gradual changes can help mitigate stress and maintain their overall health.
Feeding Recommendations
When designing a diet for an older horse, it’s important to consider factors such as body weight, activity level, and specific health conditions. Senior horses typically require a diet rich in easily digestible fiber, with added fats and proteins to compensate for their decreased digestive efficiency. Probiotics and prebiotics can also play a role in supporting gut health and improving nutrient absorption.
It’s essential to avoid feeding dusty or moldy hay, as older horses are more susceptible to respiratory issues and gastrointestinal problems. Soaking hay before feeding can help reduce dust and make it easier to chew for horses with dental issues. Additionally, complete feeds that incorporate all necessary nutrients can be an excellent option for horses that can no longer consume enough forage.
Caring for an older horse requires a holistic approach that combines tailored nutrition, careful management, and regular veterinary care. By understanding and addressing the unique needs of senior horses, owners can help their equine companions age gracefully and maintain a good quality of life. Every horse is an individual, so working closely with a veterinarian or equine nutritionist to develop a personalized care plan is essential for ensuring their long-term health.
For more detailed information on managing the nutritional needs of older horses, you can refer to resources such as OSU Extension, The Horse, Florida IFAS, and The Open Sanctuary Project.
This article originally appeared in the September 2024 issue of Oklahoma Farm & Ranch.
-
 Attractions8 years ago
Attractions8 years ago48 Hours in Atoka Remembered
-

 Country Lifestyle8 months ago
Country Lifestyle8 months agoJuly 2017 Profile: J.W. Hart
-

 Country Lifestyle9 years ago
Country Lifestyle9 years agoThe House a Treasure Built
-

 Country Lifestyle3 years ago
Country Lifestyle3 years agoThe Two Sides of Colten Jesse
-

 Outdoors7 years ago
Outdoors7 years agoGrazing Oklahoma: Honey Locust
-

 Equine8 years ago
Equine8 years agoUmbilical Hernia
-

 Outdoors5 years ago
Outdoors5 years agoPecan Production Information: Online Resources for Growers
-

 Farm & Ranch7 years ago
Farm & Ranch7 years agoHackberry (Celtis spp.)