Farm & Ranch
Cattle Nematodes (Worms)

Barry Whitworth, DVM | Senior Extension Specialist | Department of Animal & Food Sciences
According to the Mesonet, Oklahoma received some much-needed rain in late April (2023). With the moderate temperatures and high humidity, the environment is perfect for the proliferation of gastrointestinal nematodes (GIN) which are commonly called “worms.” Cattle can be infected with a variety of GIN. Most do not cause issues unless husbandry practices are poor. However certain GIN have been associated with disease. The most pathological GIN in cattle is Ostertagia ostertagi. Cooperia species and Haemonchus species are two that have been implicated with production issues. Control of these parasites is constantly changing due to environment, anthelmintic (dewormer) resistance, and consumer preference. Cattle producers should develop a plan to manage these parasites.
In order for GIN to complete their life cycle, certain environmental conditions must exist. The development stage begins with passing of the egg in the feces of the animal. If the egg is to hatch, the temperature must be warm and the humidity needs to be close to 100%. Ideal temperature ranges from 70⁰ to 80⁰ Fahrenheit (F), but any temperature above 45⁰ F will allow for development. Temperatures above 85⁰ F or below 45⁰ F will begin to hamper development. Humidity needs to be 80% or higher.
Once the egg hatches, the larva goes through a couple of molts to reach the infective stage which is the third stage larva (L3). L3 must have moisture to free itself from the fecal pat. Once free, it rides a wave of water on to a blade of forage. Once ingested, this begins the prepatent or pre-adult stage. Two molts take place during this stage (L3 to L4 and L4 to L5). If conditions are not favorable for survivability of offspring, L4 will go into an arrested development stage (hypobiosis) for a period of time. The patent or adult stage is the mature breeding adult.
Once inside the body, the parasite will migrate to certain locations in the digestive tract. For example, O. ostertagi develop in the gastric gland in the abomasum. H. placei and H. contortus will migrate to the abomasum. Cooperia species will live in the small intestine. A few like Trichuris (whipworms) are found in the large intestine.
Clinical signs of parasitism vary according to the species of parasite, burden, and site of attachment. Severe disease, which is referred to as parasitic gastroenteritis (PGE), with internal parasites is unusual with today’s control methods. Clinical signs of PGE are lack of appetite, weight loss, weakness, diarrhea, submandibular edema (bottle jaw), and death. However, most parasite infection are subclinical which means producers do not see clinical signs of disease. In subclinical infections, the parasite causes production issues such as poor weight gain in young cattle, reduced milk production, and lower pregnancy rates.
Producers should be monitoring their herds for parasites throughout the year but especially in the spring when conditions are ideal for infection. A fecal egg count (FEC) is a good way of accessing parasite burdens. Livestock producers need to gather fecal samples from their herd periodically. The samples should be sent to their veterinarian or a veterinary diagnostic lab. Different techniques are used to access the number of eggs per gram of feces. Based on the counts, the producer will learn the parasite burden of the herd. Producers can use this information to develop a treatment plan.
In the past, GIN control was simple. Cattle were routinely dewormed. Unfortunately, anthelmintic resistance has complicated parasite control. Now proper nutrition, grazing management, a general understanding of how weather influences parasites, biosecurity, refugia, anthelmintic efficiency, and the judicious use of anthelmintics are important in designing an effective parasite management program. All of these considerations need to be discussed in detail with a producer’s veterinarian when developing a plan for their operation.
Cattle producers need to understand that parasites cannot be eliminated. They must be managed with a variety of control methods. Designing a parasite management plan requires producers to gain a general understanding of life cycle of the parasite as well as the environmental needs of the parasite. Producers should use this information as well as consult with their veterinarian for a plan to manage GIN. For more information about GIN, producers should talk with their veterinarian and/or with their local Oklahoma State University Cooperative Extension Agriculture Educator.
References
Charlier, J., Höglund, J., Morgan, E. R., Geldhof, P., Vercruysse, J., & Claerebout, E. (2020). Biology and Epidemiology of Gastrointestinal Nematodes in Cattle. The Veterinary clinics of North America. Food animal practice, 36(1), 1–15.
Navarre C. B. (2020). Epidemiology and Control of Gastrointestinal Nematodes of Cattle in Southern Climates. The Veterinary clinics of North America. Food animal practice, 36(1), 45–57.
Urquhart, G. M., Armour, J., Duncan, J. L., Dunn, A. M., & Jennings, F. W. (1987). In G. M. Urquhart (Ed). Veterinary Helminthology. Veterinary Parasitology (1st ed., pp 3-33). Longman Scientific & Technical.
Farm & Ranch
Lice in Cattle

Barry Whitworth, DVM, MPH | Senior Extension Specialist
Department of Animal & Food Sciences | Freguson College of Agriculture | Oklahoma State University
Cattle lice cost Oklahoma cattlemen millions of dollars each year in decreased weight gains and reduced milk production. If cattle producers have not treated their cattle for lice this fall, they need to consider what type of lice control to initiate. This is especially true for cattle producers that had problems in the previous year. Cattle producers should monitor cattle closely during the months of December, January, and February. Producers should not wait until clinical signs appear before beginning treatment.
The life cycle of the different species of cattle lice are very similar. The life cycle begins with the female louse attaching her egg to a shaft of hair. The egg will hatch as a small replica of the adult. After several molts, the adult will emerge. The cycle takes around 3 to 4 weeks to complete. These newly hatched lice will spend their entire life on the host and are host specific which means cattle cannot be infected with lice from other animals.
Small numbers of lice may be found on cattle in the summer, but high populations of lice are associated with cold weather. Since cattle tend to be in closer proximity to each other in the winter, lice can spread easily between cattle. A small percentage of cattle tend to harbor larger numbers of lice. These animals are sometimes referred to as “carrier animals”, and they may be a source for maintaining lice in the herd. As with many other diseases, stress also contributes to susceptibility and infestation.
Signs of lice infections in cattle are hair loss, unthrifty cattle, and hair on fences or other objects. If producers find these signs, they may want to check a few animals for lice. They can check for lice by parting the hair and observing the number of lice per square inch. If an animal has 1 to 5 lice per square inch, they are considered to have a low infestation. Cattle with 6 to 10 lice would be considered moderately infested. Any cattle with more than 10 lice per square inch are heavily infested.
Cattle have two types of lice. One type is the biting or chewing louse. These lice have mouth parts that are adapted to bite and chew the skin. The second type is sucking louse. These lice have mouth parts that will penetrate the skin and suck blood and other tissue fluids. It is not uncommon for cattle to be infested with more than one species of lice.
The biting or chewing louse is Bovicola (Domalinia) bovis. This type of lice feeds on hair, skin, skin exudate, and debris. Typical clinical signs with this type of louse are hair loss, skin irritation and scabs on the skin. They are found on the shoulders and back.
Four types of sucking lice can be found in the United States. The first is the “short nose” louse or Haematopinus eurysternus. This is the largest cattle louse. This louse is found on the neck, back, dewlap, and base of the tail. The second is the “long-nose” louse or Linognathus vituli. This louse is bluish in color with a long slender head. This louse is found on the dewlap, shoulders, sides of the neck, and rump. The third is the “little blue” louse or Solenoptes cappilatus. This louse is blue in color and is the smallest cattle louse. This louse is found on the dewlap, muzzle, eyes, and neck. The last is the “tail” louse or Haematopinus quadripertuses. This louse has been found in California, Florida, and other Gulf Coast States. This louse is found around the tail.
The sucking lice have the potential to cause severe anemia if the numbers are high. This can result in poor doing cattle or in extreme cases death. They also can spread infectious diseases. The long-nose louse has been found to be a mechanical vector for anaplasmosis.
Prevention of lice infestation should begin in the fall. Producers should not wait for clinical signs to appear before beginning treatment. Several products are available to control lice. Producers should read and follow the label directions. Producers should keep in mind that many of the lice control products require two administrations to control lice. Failure to do this may result in cattle having problems with lice infestations.
Some producers have complained that some products do not work. These complaints have not been verified; however, this is a good reason to consult with a veterinarian for advice on what products to use. Most treatment failures are associated with incorrect application not resistance. Proper application of Pour-On insecticides is to administer from the withers to the tailhead. Also, the proper dose is essential for good control.
Cattle producers need to consider a few other things in lice control. Since cattle in poor body condition are more prone to lice infestation, producers need to be sure that the nutritional needs of their cattle are being met. Cattle that have a history of lice infestations should be culled. Lastly, any purchased cattle need to be inspected for lice before entering the herd. If lice are found, the animals should be isolated and treated before entering the herd.
If producers would like more information on lice in cattle, they should contact their local veterinarian or Oklahoma State University County Extension Agriculture Educator. They may also want to read Oklahoma Cooperative Extension Fact Sheet Beef Ectoparasites VTMD-7000 at https://extension.okstate.edu/fact-sheets/beef-cattle-ectoparasites.html.
Farm & Ranch
From Plow to Plentiful: The Most Important Inventions in Agricultural History
Agriculture is the foundation of human civilization. Throughout history, the quest for more efficient and productive methods of farming has led to the invention of countless tools and technologies. These inventions have not only revolutionized agriculture but have also played a pivotal role in shaping societies and economies. In this comprehensive exploration, we will delve into some of the most important inventions related to agriculture that have had a profound and lasting impact on the way we grow and harvest food.
The Wheel and Axle: Unlocking Mobility and Productivity
The wheel and axle, one of the earliest inventions in human history, had a significant impact on agriculture. This invention, which dates back to around 3500 BC, revolutionized transportation, making it possible to move heavy loads and machinery more efficiently. In agriculture, the wheel and axle played a crucial role in the development of carts, wagons, and plows, enabling farmers to transport goods and cultivate larger areas of land.
The Plow: Cultivating the Earth’s Riches
The plow is arguably one of the most iconic agricultural inventions. Its origins trace back to ancient Mesopotamia and Egypt around 3000 BC. The plow transformed agriculture by allowing farmers to dig deep furrows in the soil, turning it over and aerating it. This improved soil quality, making it more fertile and suitable for planting a wider variety of crops. The plow’s evolution from simple wooden implements to more sophisticated steel plows in the 19th century drastically increased the efficiency of farming.
Irrigation Systems: Mastering Water Management
Irrigation systems are a testament to human ingenuity in harnessing water for agriculture. The earliest known irrigation systems date back to ancient Egypt and Mesopotamia, around 6000 BC. These systems, which transported water from rivers to fields, allowed farmers to cultivate crops even in arid regions. Over time, irrigation methods have become increasingly sophisticated, incorporating canals, pumps, and drip irrigation systems, ensuring a consistent and controlled water supply for agriculture. Today, modern irrigation practices help feed billions of people around the world.
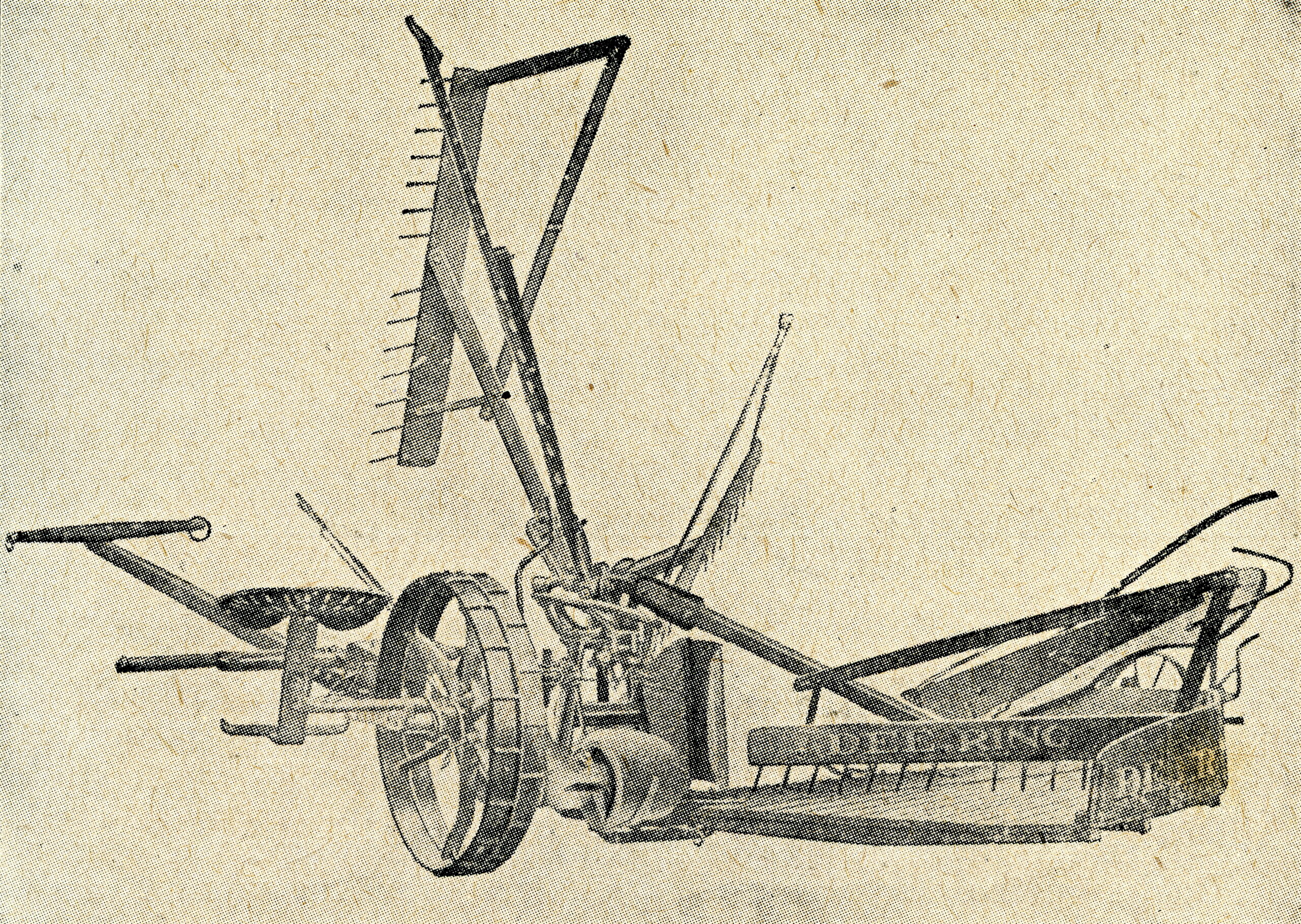
The Seed Drill: Sowing the Seeds of Precision
The seed drill, invented by Jethro Tull in the early 18th century, represented a leap forward in precision agriculture. Before its invention, seeds were sown by hand, resulting in uneven distribution and often wasteful planting practices. Tull’s seed drill, powered by horses, allowed farmers to sow seeds at a consistent depth and spacing, significantly increasing crop yields. This invention laid the groundwork for modern agricultural practices, emphasizing efficiency and precision in planting.
The Cotton Gin: Revolutionizing Textile Production
While not directly related to food production, the cotton gin, invented by Eli Whitney in 1793, had a profound impact on agriculture in the American South. This revolutionary machine automated the process of separating cotton fibers from their seeds, increasing the efficiency of cotton production by a factor of 50. The cotton gin’s success led to the widespread cultivation of cotton as a cash crop, shaping the economic landscape of the Southern United States.
The Mechanical Reaper: Harvesting the Bounty
The mechanical reaper, invented by Cyrus McCormick in the 1830s, mechanized the labor-intensive process of harvesting grain crops such as wheat. This invention featured a cutting mechanism that could efficiently harvest crops at a much faster rate than manual labor. The mechanical reaper played a pivotal role in increasing agricultural productivity during the 19th century and contributed to the expansion of agriculture in the United States.
The Steam Engine: Powering Progress
The steam engine, invented by James Watt in the late 18th century, revolutionized agriculture by providing a reliable source of power for various farming machinery. Steam engines were used to drive pumps for drainage, power threshing machines, and even locomotives for transporting agricultural goods to markets. The introduction of steam power marked a significant shift from human and animal labor to mechanical power, greatly increasing agricultural efficiency.
The Refrigerated Railcar: Expanding Food Distribution
In the late 19th century, the refrigerated railcar, often credited to Gustavus Swift, transformed the way food was transported and distributed. Before its invention, the transportation of perishable goods was a major logistical challenge. Refrigerated railcars allowed for the long-distance shipment of fresh produce, meat, and dairy products, opening up new markets and ensuring a more reliable food supply for urban populations.
Pesticides and Herbicides: Protecting Crops
The development of synthetic pesticides and herbicides in the 20th century marked a significant milestone in agriculture. These chemical compounds, such as DDT and glyphosate, helped farmers combat pests and weeds that threatened their crops. While these chemicals have played a vital role in increasing agricultural productivity, their use has also raised concerns about environmental impact and health risks, leading to ongoing debates and regulatory measures.
The Green Revolution: Feeding the World
The Green Revolution, which began in the mid-20th century, represented a coordinated effort to improve crop yields through the development of high-yielding varieties of staple crops, improved irrigation techniques, and the increased use of fertilizers and pesticides. This agricultural revolution, led by scientists like Norman Borlaug, played a pivotal role in increasing food production worldwide, helping to avert widespread famine and addressing the food needs of a growing global population.
Genetically Modified Organisms (GMOs): Customizing Crops
Genetically modified organisms (GMOs) represent a more recent innovation in agriculture. GMOs are organisms whose genetic material has been altered in a way that does not occur naturally. In agriculture, this technology has been used to develop crops with traits such as resistance to pests, tolerance to herbicides, and improved nutritional content. GMOs have sparked considerable debate over their safety, environmental impact, and ethical considerations.
Precision Agriculture: The Digital Age of Farming
The digital revolution has brought agriculture into the realm of big data and advanced technology. Precision agriculture, also known as smart farming, leverages sensors, GPS technology, drones, and data analytics to optimize various aspects of farming, including planting, irrigation, and crop management. This data-driven approach allows farmers to make informed decisions, minimize resource wastage, and increase crop yields, ultimately contributing to sustainable and efficient agriculture.
Throughout history, agriculture has been a dynamic and ever-evolving field driven by innovation and necessity. The inventions discussed in this article represent a sampling of the many remarkable contributions that have shaped the way we grow and harvest food. As we confront contemporary challenges, such as climate change, food security, and sustainable agriculture, the spirit of innovation continues to drive the development of new technologies and approaches that will shape the future of agriculture. Whether through advancements in genetic engineering, digital agriculture, or sustainable practices, the journey of agricultural innovation is far from over. As we look ahead, we can expect agriculture to continue to adapt and transform, ensuring that the world’s growing population has access to safe, nutritious, and abundant food.
Farm & Ranch
The Working Dog

By Laci Jones
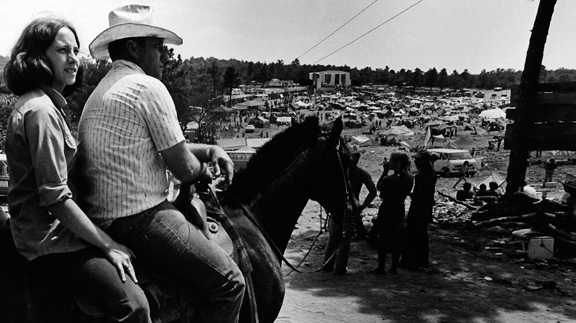
A dog is commonly referred to as “man’s best friend,” but is the saying still true for a working dog?
Randy Reed, an Oklahoma dog trainer for more than 10 years said having working dogs on the farm and ranch is helpful because of their ability to sort livestock. He said having a good working dog will make the trainer look good.
“These dogs will teach you just as much as you can teach them,” Reed said. “They are intelligent dogs, and all they want is to work and please you.”
Each dog has a different technique to herding livestock, Reed explained.
“Herding dogs were developed to do certain jobs for different types of livestock and for different types of farming,” said Susan Bennett, president of the Oklahoma Stock Dog Association.
Some dogs, known as headers, will herd livestock by putting pressure toward the stock’s head. Other dogs, known as heelers, will nip at the heels of stock to herd them. Bennett said some dogs can be headers and heelers. Each livestock species may require a different approach, Reed said.
“Working sheep is different than working cattle,” he said. “The dogs can work the sheep with their eyes. You don’t have to be on sheep so tight, but it’s a challenge with cattle.”
For an owner, it may be a challenge to decide which dog breed is appropriate to have. The best working dog breed depends on what livestock species is worked and the owner’s preferences.
Border Collie
Border collies are known for their herding ability, Bennett said. This breed of dog was bred for their intelligence and work ethic.
“The border collies that actually work livestock were never bred for how they looked,” she added.
Border collies typically use their eyes to herd livestock, but they can also be sent into a pasture and gather livestock.
“If you want to pull 300 yearlings off of a wheat pasture, you can pull up to the gate send the border collies out there,” Reed said. “They will bring the cattle right to you and through the gate.”
Bennett said people need to make sure they have jobs for working dogs.
“These dogs have been bred for hundreds of years, and they have to find an outlet for that instinct,” Bennett said.
When the border collies are not working, both Bennett and Reed keep their border collies in pens.
“I can run them loose, but they will overwork the stock,” Reed said. “They are like keeping an eye on kids.”
A downside to having a border collie is some may not have a tough enough bite, Reed said. They may not be as aggressive as other dog breeds.
Kelpie
Kelpies originated from Australia and are typically short, slick-haired dogs. This breed of dog is rangier than most other breeds, Reed said.
“Kelpies’ working style is similar to border collies,” he said.
Like border collies, kelpies are a “fetch” dog, meaning they will bring the livestock back to the owner, he said.
Bennett said the kelpies she has seen are typically more aggressive toward livestock. They have more stamina than most breeds, Reed added.
“When they go to work, they will be in a crouch position,” Reed said. “Their head is going to be down level with their shoulders. The tail is going to be dropped down behind them.”
Good border collies and kelpies have constant control, and they will have a lot of movement with their eyes, he said.
Reed said the American kelpie is close in proximity with the Australian kelpie. However, the American kelpie is weaker than the Australian kelpie.
Australian Cattle Dog
Developed from the native Australian dingo, the Australian cattle dogs was originally bred for driving livestock, Bennett said.
She said most working dogs within this breed are heelers, which is why they are commonly referred to as blue or red heelers, depending on their color.
Australian cattle dogs are typically used in pens and corrals to move livestock, Bennett said. They were not developed to go into open areas and gather livestock.
“We would haul cattle to the sale barn,” Reed said. “There was a blue heeler that would work on the chute and bite the cattle and get them through there.”
However, the Australian cattle dog is not as common in the competition trials as the border collie.
Reed said there is a market for the Australian cattle dog in the state. Australian cattle dogs are in high demand, but their herding ability is still to be determined.
Australian Shepherd
“Back when the United States was being settled, the Australian shepherd was the farm dog to have,” Bennett said.
Bennett said Australian shepherds were bred to be farm dogs, but they have changed in recent years to become show dogs and pets.
“There are very few Australian shepherds that can now go out and do a job,” Bennett said.
The Australian shepherd is not as popular for herding as other breeds today, Reed added.
“They are pretty dogs, but I haven’t seen any stock-oriented,” Reed said.
Reed said Australian shepherds can be trained, but he found them to be easily distracted.
Catahoula
Catahoulas are typically used for hunting. However, these bay-type dogs can be used to work livestock.
Reed said catahoulas and border collies have different styles of working. Unlike the border collie, this breed of dog uses their bark to move livestock, Reed said. Catahoulas will also work the outer perimeter of livestock, he said.
“Catahoulas will hunt livestock because they can use their nose, where the border collie will do everything by the power of their eyes,” Reed said.
Reed said catahoulas would be the better working dog in a situation where the owner needed help finding livestock.
However, working livestock with a catahoula is a team effort. A catahoula dog will not fetch livestock, but they will keep livestock in a “tight wad.” The owner will have to move the cattle themselves.
Cattlemaster
The cattlemaster is a newer breed of working dog. They are a cross between Border collie, pit bull, and kelpie, and they were bred for working cattle, according to Reed. They are more aggressive and have a stronger bite.
However, when cattlemaster was bred to get more bite, they lost their natural herding ability. Reed experienced this firsthand when he trained a cattlemaster.
“There wasn’t the natural ability,” Reed said. “She was just mechanical. I can move her, but she couldn’t read a cow.”
Reed said other breeds of dogs can potentially be used as working dogs including corgis, McNab shepherds and German shepherds. However, before purchasing a new dog, the buyer should research bloodlines and breeders.
“Buy a dog that can be bred to work cattle,” Reed advised. “Go watch the parents work and research who has trained the dogs.”
It is also important to purchase a dog that has been bred to work the specific species of livestock, Bennett added. No matter what dog breed an owner chooses, imported dogs may not always make the best working dogs.
“Just because a dog is imported doesn’t mean it will be better than a dog bred right here in the United States,” Bennett said.
She said there are many more great dogs and trainers in the United States than 20 years ago. It may be helpful to seek advice from a professional to help kick-start a new program, she added.
After purchasing a working dog, it is important to spend extra money to send the dog to a trainer for 30 to 60 days, Reed said. Then, the owner should spend quality time with the dog and the trainer to learn how to work together.
Bennett said each dog may require a different type of training, which may require adjusting. She said incorporating techniques from several different trainers can help the owner and their best friend.
This article was originally published in the January 2016 edition of Oklahoma Farm & Ranch.
-
 Attractions8 years ago
Attractions8 years ago48 Hours in Atoka Remembered
-

 Country Lifestyle7 months ago
Country Lifestyle7 months agoJuly 2017 Profile: J.W. Hart
-

 Country Lifestyle9 years ago
Country Lifestyle9 years agoThe House a Treasure Built
-

 Country Lifestyle3 years ago
Country Lifestyle3 years agoThe Two Sides of Colten Jesse
-

 Outdoors7 years ago
Outdoors7 years agoGrazing Oklahoma: Honey Locust
-

 Outdoors5 years ago
Outdoors5 years agoPecan Production Information: Online Resources for Growers
-

 Equine7 years ago
Equine7 years agoUmbilical Hernia
-

 Farm & Ranch6 years ago
Farm & Ranch6 years agoHackberry (Celtis spp.)